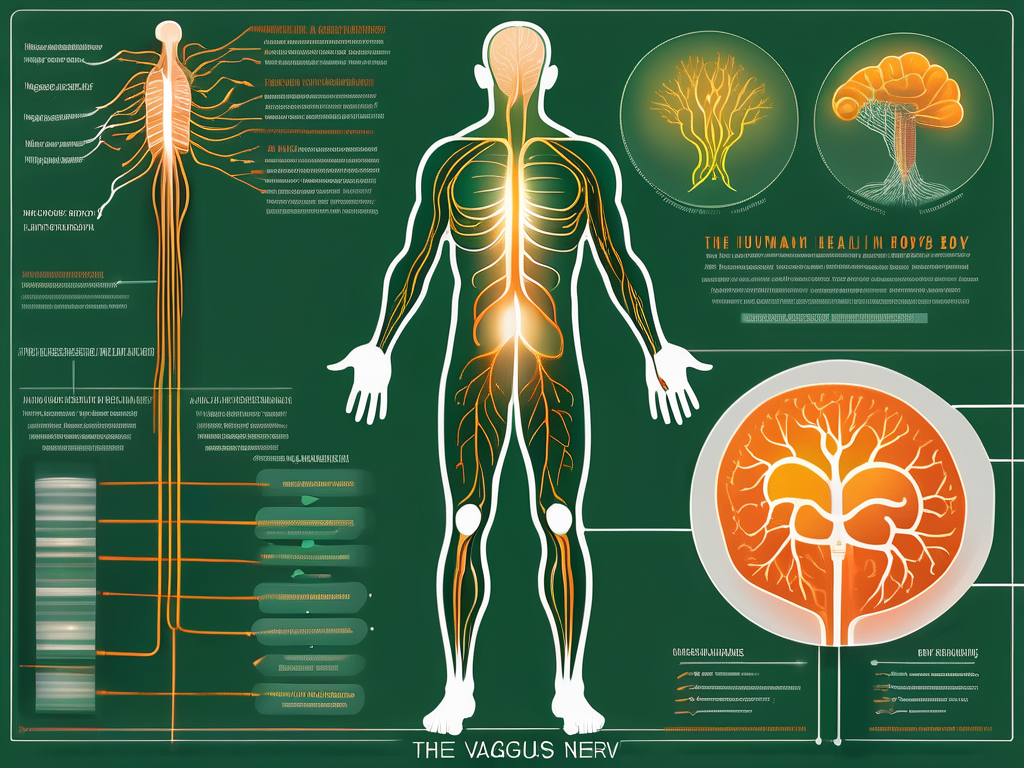
Das Fasten und der Vagusnerv: Eine Verbindung zur Gesundheit

Erfahren Sie, wie das Fasten und der Vagusnerv miteinander verbunden sind und welche Auswirkungen dies auf die Gesundheit haben kann.
Stimulation des Vagusnervs: Eine wirksame Methode zur Verbesserung der Gesundheit
Erfahren Sie, wie die Stimulation des Vagusnervs Ihre Gesundheit verbessern kann.
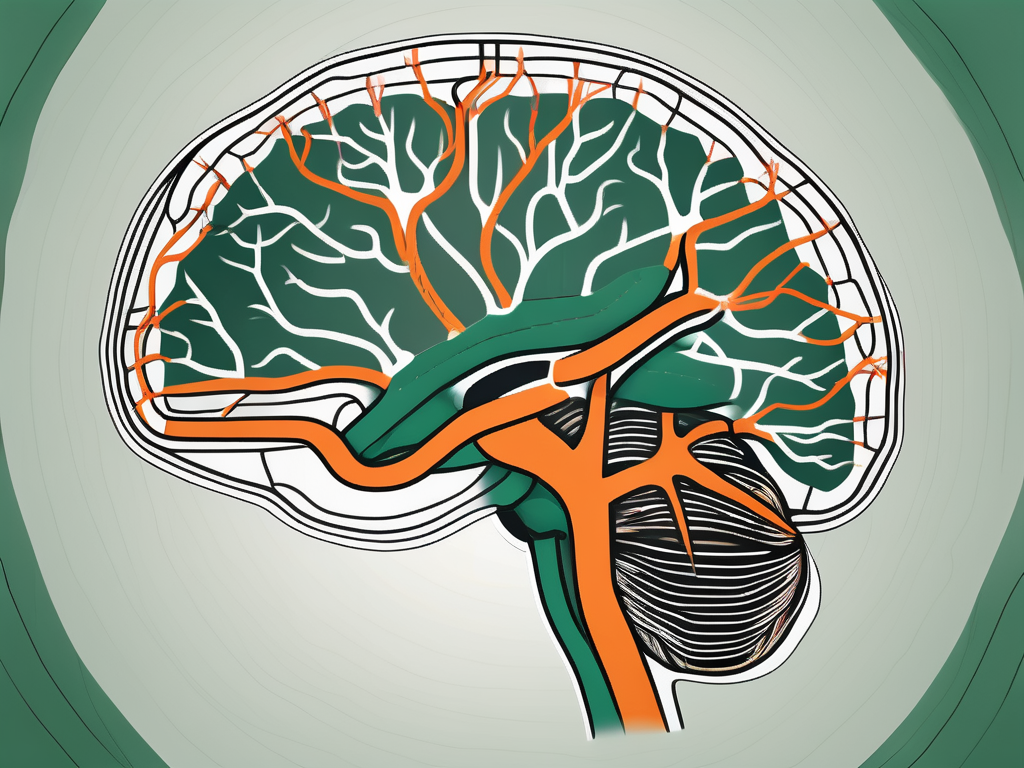
Der Vagusnerv: Funktionen und Bedeutung auf Deutsch
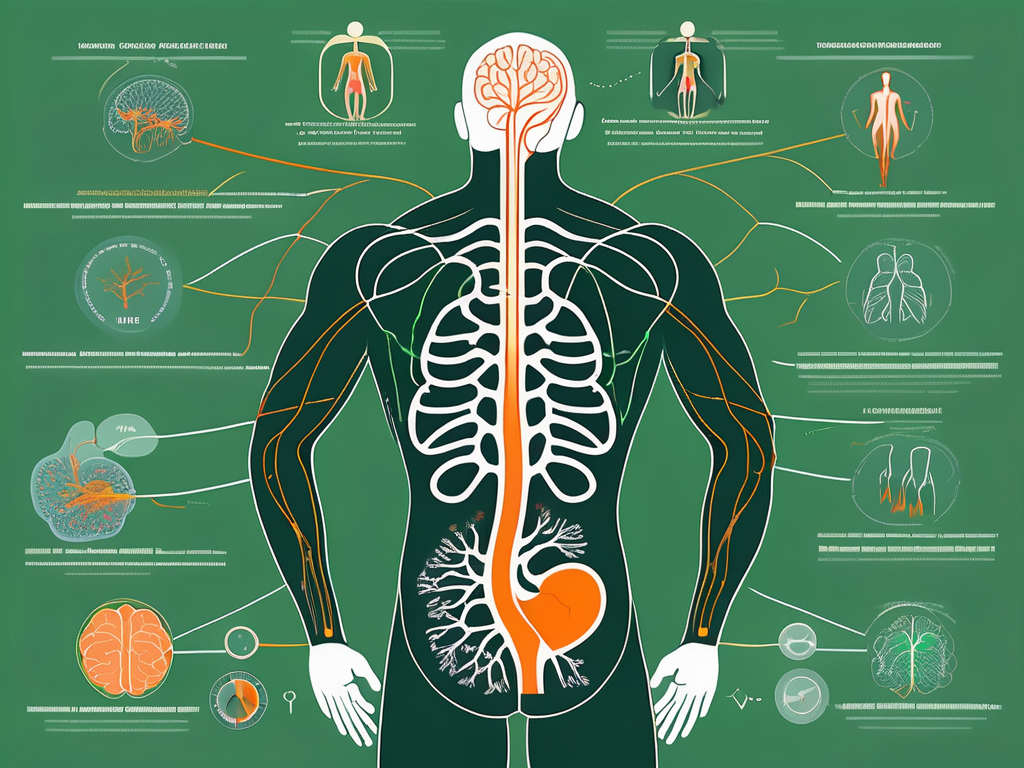
Erfahren Sie alles über den Vagusnerv und seine vielfältigen Funktionen in unserem informativen Artikel.
Osteopathie und der Vagusnerv: Eine ganzheitliche Verbindung

Erfahren Sie, wie die Osteopathie und der Vagusnerv eine ganzheitliche Verbindung eingehen.
Die Bedeutung des Apollo-Nervs für die Gesundheit: Eine umfassende Untersuchung

Erfahren Sie in diesem umfassenden Artikel über die Bedeutung des Apollo-Nervs für die Gesundheit.
Die Bedeutung der Vagusatmung für die Gesundheit

Erfahren Sie in diesem faszinierenden Artikel die Bedeutung der Vagusatmung für Ihre Gesundheit.
Der Vagusnerv: Stressabbau und Entspannungstechniken

Erfahren Sie in unserem Artikel “Der Vagusnerv: Stressabbau und Entspannungstechniken” alles über die faszinierende Rolle des Vagusnervs bei der Stressbewältigung und welche effektiven Entspannungstechniken Sie zur Aktivierung dieses “Wundernervs” nutzen können.
Die Auswirkungen des Vagusnervs auf Migräne: Eine umfassende Analyse
Erfahren Sie in diesem umfassenden Artikel, wie der Vagusnerv die Migräne beeinflusst.
Erleben Sie eine einzigartige Sinnesreise im Nocti Vagus Dunkelrestaurant & Dunkelbühne

Erleben Sie eine faszinierende Sinnesreise im Nocti Vagus Dunkelrestaurant & Dunkelbühne.
Die Bedeutung des Vagusnervs für das Wohlbefinden: Eine Untersuchung von Sukie Baxter

Erfahren Sie in diesem faszinierenden Artikel die Bedeutung des Vagusnervs für Ihr Wohlbefinden, basierend auf der Untersuchung von Sukie Baxter.


