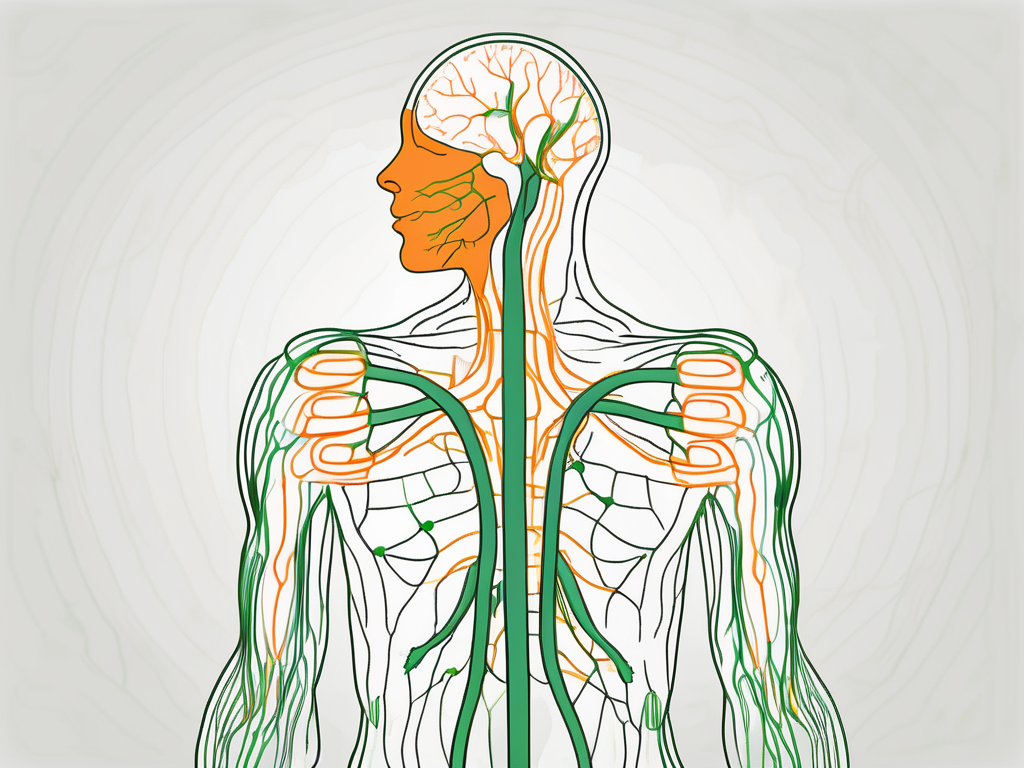
Where Is the Vagus Nerve Located in the Neck?

Discover the exact location of the vagus nerve in the neck and its crucial role in regulating essential bodily functions.
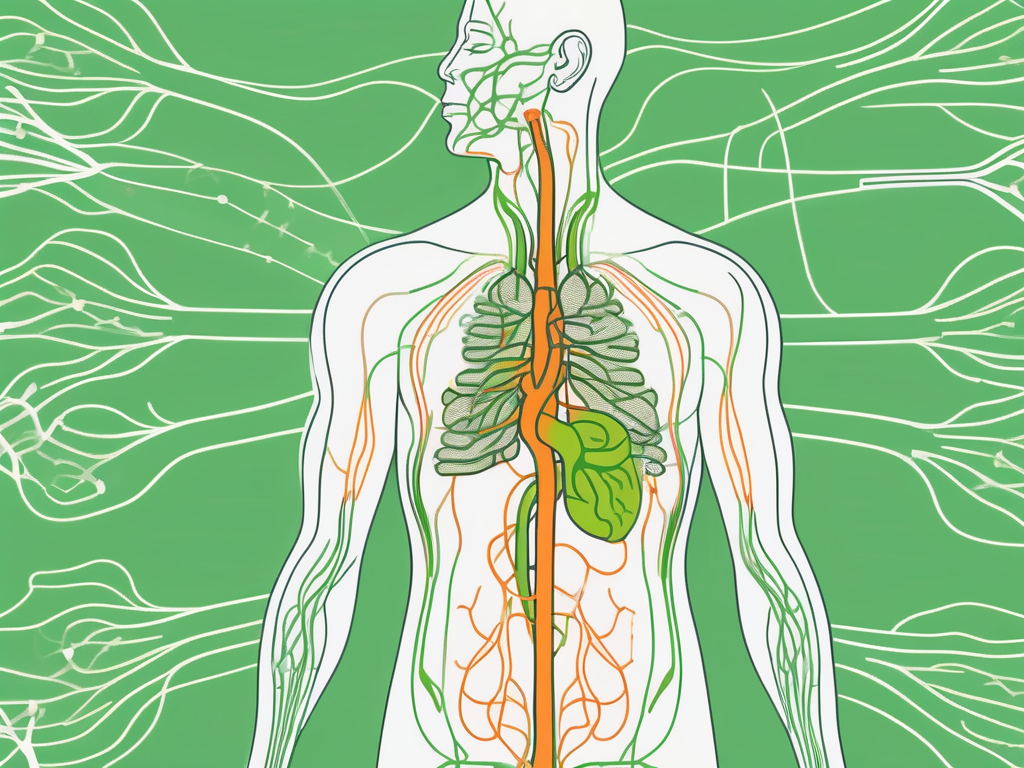
Boost Digestion with Vagus Nerve Exercises in 5 Easy Steps

Learn how to improve your digestion with simple vagus nerve exercises in just 5 easy steps.
Applying Acupuncture for Carpal Tunnel Syndrome

Discover the ancient practice of acupuncture and how it can provide relief for carpal tunnel syndrome.
Best Measure of Pain Modulation Effects: Exploring Effective Strategies

Discover the most effective strategies for measuring pain modulation effects in this comprehensive article.
Applying Aromatherapy for Anxiety Relief

Discover how to effectively use aromatherapy for anxiety relief.
Applying Acupuncture for Arthritis

Discover the ancient practice of acupuncture and its potential benefits for arthritis relief.
Can a Urinary Tract Infection Trigger Vagal Tone Increase?
Discover the potential connection between urinary tract infections and vagal tone increase in this intriguing article.
Can Vagus Nerve Stimulation Cause Coughing?
Discover the surprising connection between vagus nerve stimulation and coughing in this insightful article.
Increase Vagal Tone at Night: Essential Tips for Better Health

Discover essential tips to increase vagal tone at night and improve your overall health.
Can Increased Vagal Tone Cause Excess Salivation?

Discover the link between increased vagal tone and excess salivation in this comprehensive article.


