Understanding tVNS: Parameters and Applications – An Overview

Transcutaneous Vagus Nerve Stimulation (tVNS) is a non-invasive form of nerve stimulation that has been shown to have a range of potential therapeutic applications. By stimulating the vagus nerve, tVNS can modulate a variety of physiological processes, including inflammation, pain, heart rate, blood pressure, digestion and more. In this article, we’ll take a look […]
The Optic Nerve
The second cranial nerve, or optic nerve (CN II), is in charge of carrying unique relevant stimuli for vision. It originates from the optic vesicle, a forebrain out pocketing. Since the optic nerve is a vital part of the central nervous system, its examination permits the evaluation of the intracranial environment. The cranial meninges are […]
Gastroparesis – Symptoms, Treatment, and Vagus Nerve Stimulation

As you probably know, eating is one of the essential things in life. The ability to enjoy food often keeps us going when we’re feeling down or stressed out, and it can be a source of joy and comfort. However, eating can become frustrating and unpleasant if you have gastroparesis or another digestive disorder affecting […]
The Cranial Nerves

The cranial nerves are made up of twelve pairs of nerves with the origin at the back of the brain while passing the spinal cord (1). The cranial nerves serve as a connection between the brain and other parts of the body performing sensory and motor functions. The sensory functions are responsible for the sense […]
What Is Heart Rate Variability?
What makes the heart rate and its variability very unique? Heart rate variability simply means the measure of the variation in the time interval between each heartbeat in milliseconds. These fluctuations are usually undetectable except with specialized devices. This measure can be a sign of your overall health and well-being. HRV measures how uneven your […]
Current Control or Voltage Control?
Current control or Voltage control – what’s the difference, really? What is the difference between a voltage control and current controlled stimulator? We often get asked to explain the difference between a tens device – which is a voltage controlled output and our tVNS which is a current controlled output. They sound the same so […]
Where is the Vagus Nerve?
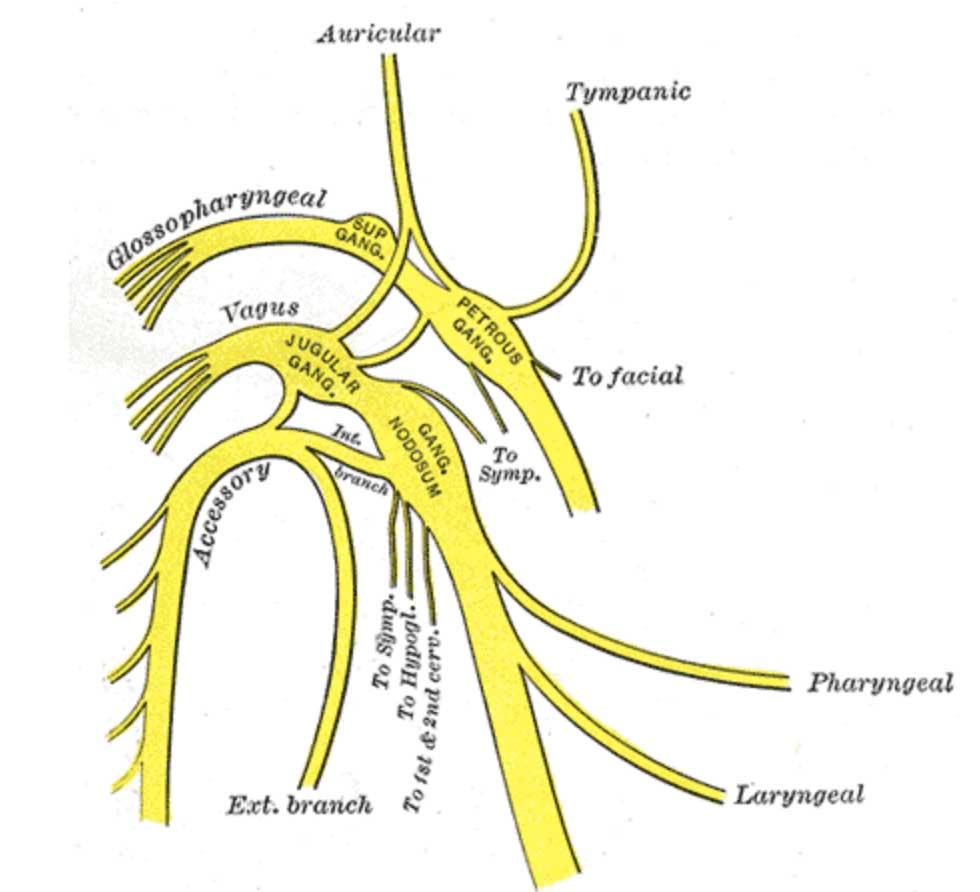
Vagus Nerve Anatomy-Where is the Vagus Nerve? Nerves play a very important role in our body. Nerves form the basis of message conduction in the body. Some take messages from the brain to the body via spinal cord and some nerve fibers are responsible for conducting messages from the body parts like organs to the […]
Vagus Nerve Damage Testing

There are various ways in which the vagus nerve can be tested as it innervates and controls many functions in the body. Before we can talk about the vagus nerve damage test, we need to learn what the nervous system is and the functions of the vagus nerve. The nervous system is the connecting network […]
The Vagus Nerve and Its Role in Healthy Living

If you’ve just heard of the vagus nerve and you’re wondering what it is and why people are talking so much about it, you’ve come to the right place. This article will give you an overview of what the vagus nerve is and why it is considered so important to health and well being. Recent […]
Heart Rate Variability and Why You Should Care
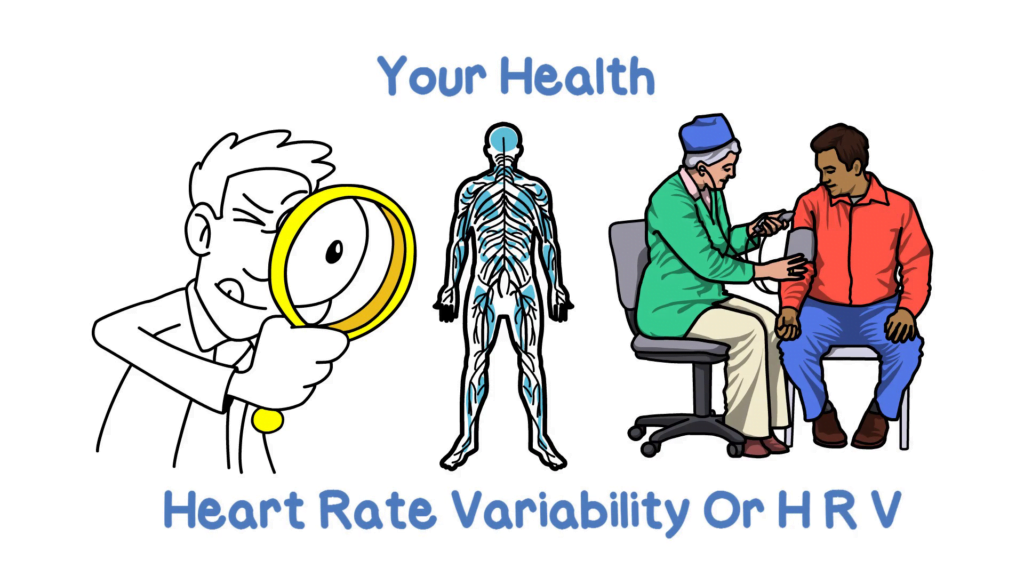
We used to think we could measure our circulatory health with a combination of blood pressure and heart rate. Low measures indicated healthy arteries, veins, and heart. However, recently researchers have begun to realize that there is another interesting and powerful measure of the strength of your nervous and circulatory systems and of your health […]


